INTRODUCTION
Diabetes mellitus, commonly referred to as diabetes, is a metabolic disorder characterized by high blood sugar levels over a prolonged period of time. It occurs when the pancreas fails to produce enough insulin, or when the body is unable to use the insulin that is produced effectively.
Insulin is a hormone that helps regulate blood sugar levels by allowing glucose to enter the body's cells, where it can be used for energy. In people with diabetes, the lack of insulin or the body's inability to use it properly causes glucose to accumulate in the blood, leading to a variety of complications.
In this blog, we will discuss the causes, symptoms, and treatments of diabetes.
TYPES OF DIABETES
There are several types of diabetes, including:
Type 1 diabetes:
This type of diabetes occurs when the immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas, leading to a deficiency of insulin. It typically develops in childhood or adolescence and requires lifelong insulin therapy.
Type 2 diabetes:
This is the most common type of diabetes and occurs when the body becomes resistant to insulin or does not produce enough of it to properly regulate blood sugar levels. It can develop at any age but is most common in adults.
Gestational diabetes:
This type of diabetes develops during pregnancy and typically resolves after delivery. Women who develop gestational diabetes have an increased risk of developing type 2 diabetes later in life.
LADA (Latent Autoimmune Diabetes in Adults):
This is a form of type 1 diabetes that develops in adults, typically over the age of 30. It progresses more slowly than typical type 1 diabetes but still requires insulin therapy.
MODY (Maturity Onset Diabetes of the Young):
This is a rare genetic form of diabetes that is usually diagnosed in childhood or adolescence. It is caused by mutations in specific genes and is inherited in an autosomal dominant pattern.
Secondary diabetes:
This type of diabetes is caused by other medical conditions or medications that affect insulin production or use. Examples include cystic fibrosis-related diabetes and steroid-induced diabetes.
However, Type 1 diabetes and Type 2 diabetes are the main subtypes of Diabetes mellitus
PREDIABETES
Prediabetes is a condition in which blood sugar levels are higher than normal, but not high enough to be classified as diabetes. It is a warning sign that a person is at risk of developing type 2 diabetes and other health problems, such as heart disease and stroke.
Prediabetes is often referred to as impaired glucose tolerance (IGT) or impaired fasting glucose (IFG), depending on the method used to diagnose it. IGT is diagnosed through an oral glucose tolerance test, while IFG is diagnosed through a fasting blood glucose test.
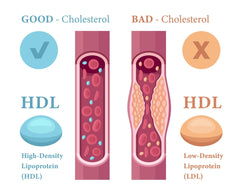
Risk factors for prediabetes include being overweight or obese, having a family history of diabetes, being physically inactive, and having high blood pressure or abnormal cholesterol levels.
The good news is that prediabetes can often be reversed through lifestyle changes such as weight loss, healthy eating, and regular physical activity. If left untreated, however, prediabetes can progress to type 2 diabetes and increase the risk of complications such as nerve damage, kidney disease, and blindness. Therefore, it is important to get tested for prediabetes and take steps to prevent or delay the onset of type 2 diabetes.
SYMPTOMS OF DIABETES
The symptoms of diabetes can vary depending on the type of diabetes and how advanced it is.
General symptoms
Common symptoms of both type 1 and type 2 diabetes include:
- Frequent urination
- Increased thirst
- Fatigue
- Blurred vision
- Slow healing of wounds
- Tingling or numbness in the hands or feet
- Weight loss
In type 1 diabetes, symptoms usually develop quickly and can be severe, while in type 2 diabetes, symptoms may develop gradually and may not be noticeable at first. It is important to note that some people with type 2 diabetes may not experience any symptoms, particularly in the early stages of the disease. Therefore, regular check-ups with a healthcare provider are recommended for early detection and management of diabetes.
Symptoms in men
There are some symptoms other than the general ones that are more common or pronounced in men, including:
- Erectile dysfunction (ED): High blood sugar levels can damage blood vessels and nerves that control sexual function, leading to difficulty achieving or maintaining an erection.
- Low testosterone levels: Men with diabetes are more likely to have low levels of the hormone testosterone, which can cause decreased libido, fatigue, and muscle weakness.
- Decreased muscle mass: Diabetes can cause muscle loss and weakness, particularly in older men.
- Bladder problems: High blood sugar levels can damage nerves that control bladder function, leading to urinary incontinence or other bladder problems.
- Poor sleep: Diabetes can disrupt sleep patterns, leading to difficulty falling or staying asleep, and causing daytime fatigue.
It is important to note that not all men with diabetes will experience these symptoms, and some men may have other symptoms not listed here. If you experience any of these symptoms, it is important to speak with a healthcare provider for proper diagnosis and treatment.
Symptoms in women
The symptoms of diabetes in women can be similar to those in men, but there are also some symptoms that are more common in women. Here are some of the symptoms of diabetes that women may experience:
- Urinary tract infections: Women with diabetes are at higher risk for urinary tract infections (UTIs) due to high blood sugar levels that can promote bacterial growth in the urinary tract.
- Yeast infections: Women with diabetes are also more prone to yeast infections, which can occur in the genital area, mouth, and skin folds.
- Polycystic ovary syndrome (PCOS): Women with diabetes are more likely to develop PCOS, a hormonal disorder that can cause irregular periods, acne, excess hair growth, and weight gain.
- Sexual dysfunction: Diabetes can also affect sexual function in women, leading to decreased sex drive, vaginal dryness, and difficulty achieving orgasm.
- Menstrual irregularities: Women with diabetes may also experience menstrual irregularities, such as missed periods or heavier-than-normal bleeding.
- Skin changes: Women with diabetes may experience skin changes, such as dry, itchy skin or dark patches on the skin, especially around the neck and underarms.
It's important to note that not all women with diabetes will experience these symptoms, and some women may not have any symptoms at all. However, if you are experiencing any of these symptoms or have any concerns about your health, it's important to speak with your healthcare provider.
Gestational diabetes
It is important to monitor and manage gestational diabetes because it can cause complications for both the mother and the baby. It's important to note that many women with gestational diabetes may not have any symptoms at all, which is why it's important to get tested for gestational diabetes during pregnancy. Here are some symptoms of gestational diabetes that women may experience:
- Increased thirst and frequent urination: Women with gestational diabetes may feel thirstier than usual and need to urinate more often.
- Blurred vision: High blood sugar levels can cause temporary changes to vision.
- Nausea and vomiting: Some women with gestational diabetes may experience nausea and vomiting, particularly in the first trimester.
CAUSES AND RISK FACTORS OF DIABETES
Each type of diabetes has a different cause associated with it.
Type 1 diabetes
The exact cause of type 1 diabetes is not fully understood, but it is believed to be a combination of genetic and environmental factors.
- Genetic factors: Type 1 diabetes has a strong genetic component, and it tends to run in families. Studies have identified several genes that are associated with an increased risk of developing type 1 diabetes. However, not everyone with these genes will develop the disease, indicating that there are other factors involved.
- Environmental factors: Environmental factors may trigger the development of type 1 diabetes in people who are genetically predisposed to the disease. Some possible environmental triggers include viral infections, particularly enteroviruses, which may damage the pancreas and trigger an autoimmune response, and early exposure to cow's milk or gluten, which may also trigger an immune response.
Type 2 diabetes
There are several factors that can contribute to the development of type 2 diabetes, including:
- Genetic factors: Type 2 diabetes has a strong genetic component, and it tends to run in families. If a person has a family history of type 2 diabetes, they are at higher risk of developing the disease.
- Obesity and sedentary lifestyle: Being overweight or obese is a major risk factor for type 2 diabetes, particularly if the excess weight is carried around the abdomen. A sedentary lifestyle, with little or no physical activity, can also increase the risk of developing type 2 diabetes.
- Insulin resistance: Insulin resistance occurs when the body's cells become less responsive to insulin, which is the hormone that regulates blood sugar levels. This can lead to higher levels of glucose in the blood and an increased risk of developing type 2 diabetes.
- Metabolic syndrome: Metabolic syndrome is a cluster of conditions that includes high blood pressure, high blood sugar, abnormal cholesterol levels, and excess body fat around the waist. People with metabolic syndrome are at increased risk of developing type 2 diabetes.
- Age and ethnicity: The risk of developing type 2 diabetes increases with age, particularly after the age of 45. Certain ethnic groups, including African Caribbean, and South Asians, are also at higher risk of developing type 2 diabetes.
Type 1.5 diabetes
Type 1.5 diabetes, also known as Latent Autoimmune Diabetes in Adults (LADA), is a form of diabetes that shares characteristics of both type 1 and type 2 diabetes. The exact cause of type 1.5 diabetes is not fully understood. Some of the factors that can contribute to the development of type 1.5 diabetes include:
- Genetics: Like type 1 and type 2 diabetes, genetics play a role in the development of type 1.5 diabetes. People with a family history of autoimmune diseases or type 1 diabetes may be at higher risk of developing type 1.5 diabetes.
- Autoimmune response: In type 1.5 diabetes, the immune system mistakenly attacks the insulin-producing cells in the pancreas, leading to a gradual loss of insulin production. This autoimmune response is similar to the one that occurs in type 1 diabetes.
- Insulin resistance: Some people with type 1.5 diabetes may also have insulin resistance, which is a characteristic of type 2 diabetes. This can make it more difficult to manage blood sugar levels.
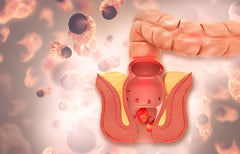
Gestational diabetes
The exact cause of gestational diabetes is not fully understood, but it is believed to be related to hormonal changes that occur during pregnancy. During pregnancy, the placenta produces hormones that can interfere with the body's ability to use insulin effectively, leading to insulin resistance and high blood sugar levels.
Some of the factors that can increase the risk of developing gestational diabetes include:
- Family history: Women with a family history of type 2 diabetes or gestational diabetes are at higher risk of developing gestational diabetes themselves.
- Overweight or obesity: Women who are overweight or obese before pregnancy are at higher risk of developing gestational diabetes.
- Age: Pregnant women who are over the age of 30 are at higher risk of developing gestational diabetes.
- Ethnicity: Certain ethnic groups, including African Americans, Hispanic/Latino Americans, Native Americans, and Asian Americans, are at higher risk of developing gestational diabetes.
- Previous gestational diabetes: Women who have had gestational diabetes in a previous pregnancy are at higher risk of developing it again.
- Polycystic ovary syndrome (PCOS): Women with PCOS, a condition that affects hormone levels and can lead to insulin resistance, are at higher risk of developing gestational diabetes.
Overall, hormonal changes during pregnancy, combined with other risk factors, can increase a woman's risk of developing gestational diabetes.
It's important to note that diabetes is a complex disease that can be influenced by a variety of factors, including genetics, lifestyle, and environmental factors. While some risk factors for diabetes cannot be controlled, such as family history and genetics, there are many lifestyle factors that can help reduce the risk of developing diabetes, such as maintaining a healthy weight, getting regular physical activity, and eating a healthy diet.
DIABETES COMPLICATIONS
If left untreated or poorly managed, diabetes can lead to a range of complications affecting different parts of the body. Here are some of the most common complications associated with diabetes:
- Cardiovascular disease: People with diabetes are at increased risk of developing cardiovascular disease, which includes conditions such as coronary artery disease, heart attack, and stroke.
- Nerve damage (neuropathy): High blood sugar levels over time can damage the nerves throughout the body, leading to symptoms such as numbness, tingling, and pain, particularly in the hands and feet.
- Kidney damage (nephropathy): Diabetes can damage the blood vessels in the kidneys, leading to kidney damage and even kidney failure in severe cases.
- Eye damage (retinopathy): High blood sugar levels over time can damage the blood vessels in the retina, leading to vision problems and even blindness.
- Foot damage: Nerve damage and poor blood flow to the feet can increase the risk of foot ulcers and infections, which can lead to amputation in severe cases.
- Skin conditions: Diabetes can cause skin conditions such as bacterial and fungal infections, as well as dry skin and itching.
- Dental problems: People with diabetes are at higher risk of developing gum disease and other dental problems.
- Depression: People with diabetes are more likely to experience depression than those without diabetes.
Gestational diabetes
Gestational diabetes can increase the risk of several complications for both the mother and the baby. Here are some of the most common complications associated with gestational diabetes:
- High birth weight: Babies born to mothers with gestational diabetes may be larger than average (macrosomia), which can increase the risk of difficult delivery, injury during delivery, and the need for a cesarean section.
- Preterm birth: Women with gestational diabetes are at higher risk of delivering prematurely (before 37 weeks).
- Low blood sugar (hypoglycemia): Babies born to mothers with gestational diabetes may experience low blood sugar levels after birth, which can cause seizures or other complications.
- Respiratory distress syndrome: Babies born to mothers with gestational diabetes may be at higher risk of developing respiratory distress syndrome, a condition that affects breathing.
- Type 2 diabetes: Women who develop gestational diabetes are at higher risk of developing type 2 diabetes later in life.
- Preeclampsia: Women with gestational diabetes are at higher risk of developing preeclampsia, a serious condition characterized by high blood pressure and damage to organs such as the kidneys and liver.
- Future pregnancy complications: Women who have had gestational diabetes in a previous pregnancy are at higher risk of developing it again in future pregnancies, and may be at higher risk of other pregnancy complications such as high blood pressure.
Overall, proper management and treatment of diabetes, including monitoring blood sugar levels, following a healthy diet, getting regular exercise, and taking medications as prescribed, can help reduce the risk of developing these complications. It is important for people with diabetes to work closely with their healthcare team to develop a personalized treatment plan and to receive regular check-ups to monitor their overall health.
TREATMENT OF DIABETES
The treatment of diabetes depends on the type of diabetes and how advanced it is.
Type 1 and 1.5 diabetes
The mainstay of treatment for type 1 and type 1.5 diabetes is insulin replacement therapy, which involves taking insulin through injections or an insulin pump. The goal of insulin therapy is to mimic the natural insulin secretion of the pancreas and keep blood sugar levels within a normal range. The amount of insulin required will depend on various factors such as age, weight, diet, and physical activity.
People with type 1 and type 1.5 diabetes may also benefit from working with a diabetes educator or healthcare team to learn how to manage their condition effectively and prevent complications. In some cases, people with type 1 diabetes may be eligible for islet cell or pancreas transplantation, although these procedures are not suitable for everyone and carry their own risks and benefits.
Type 2 diabetes
The treatment for type 2 diabetes typically involves a combination of lifestyle changes and medications. The goals of treatment are to lower blood sugar levels, manage symptoms, and prevent or delay complications associated with the disease.
Here are some common treatments for type 2 diabetes:
- Lifestyle changes: Losing weight, increasing physical activity, and following a healthy diet can help improve blood sugar control and reduce the risk of complications.
- Oral medications: There are several classes of oral medications that can help lower blood sugar levels in people with type 2 diabetes. These medications work in different ways and may be used alone or in combination with other medications.
- Injectable medications: Injectable medications such as GLP-1 receptor agonists and insulin may be used to help manage blood sugar levels in people with type 2 diabetes.
- Blood sugar monitoring: Regular blood sugar monitoring is important to help track blood sugar levels and adjust treatment as needed.
- Management of other health conditions: People with type 2 diabetes may also need to manage other health conditions such as high blood pressure, high cholesterol, and kidney disease.
- Bariatric surgery: In some cases, bariatric surgery may be recommended for people with type 2 diabetes who are severely obese and have not been able to manage their blood sugar levels through other means.
Gestational diabetes
The treatment for gestational diabetes typically involves a combination of lifestyle changes and medications to manage blood sugar levels and prevent complications during pregnancy. Here are some common treatments for gestational diabetes:
- Blood sugar monitoring: Regular blood sugar monitoring is important to help track blood sugar levels and adjust treatment as needed. This may involve monitoring blood sugar levels before and after meals, as well as before bed.
- Healthy diet: Following a healthy diet that is low in sugar and refined carbohydrates can help manage blood sugar levels and prevent complications.
- Physical activity: Regular physical activity can help lower blood sugar levels and improve insulin sensitivity.
- Medications: In some cases, medications such as insulin or oral medications may be needed to help manage blood sugar levels during pregnancy.
- Fetal monitoring: Regular fetal monitoring may be necessary to ensure that the baby is growing and developing properly.
Diet and exercise for diabetes
Diet and exercise are important components of managing diabetes and can help improve blood sugar control, prevent complications, and improve overall health. Here are some guidelines for diet and exercise for treating diabetes:
Diet:
- Choose complex carbohydrates: Complex carbohydrates are broken down more slowly by the body, which can help prevent spikes in blood sugar levels. Examples include whole grains, fruits, and vegetables.
- Avoid sugary and processed foods: Foods that are high in sugar and processed foods should be avoided or limited.
- Eat a balanced diet: A balanced diet that includes a variety of foods can help ensure that the body is getting all the nutrients it needs.
- Monitor portion sizes: Eating too much of any type of food can cause blood sugar levels to rise, so it's important to monitor portion sizes.
- Work with a registered dietitian: A registered dietitian can help develop a personalized meal plan that takes into account individual needs, preferences, and medical history.
- Aim for at least 30 minutes of moderate-intensity exercise most days of the week: Examples of moderate-intensity exercise include brisk walking, cycling, swimming, and dancing.
- Incorporate strength training: Strength training can help improve insulin sensitivity and blood sugar control.
- Monitor blood sugar levels before and after exercise: Blood sugar levels may need to be monitored before and after exercise, and adjustments may need to be made to diet or medication.
- Work with a healthcare provider: A healthcare provider can help develop an exercise plan that takes into account individual needs, preferences, and medical history.
DIABETES DIAGNOSIS
Diabetes is typically diagnosed using a combination of blood tests and symptoms. It's recommended that individuals with risk factors, such as a family history of diabetes or obesity, be screened regularly.
- Fasting plasma glucose test: This test measures blood sugar levels after an overnight fast. A level of 126 milligrams per deciliter (mg/dL) or higher on two separate occasions is indicative of diabetes.
- Oral glucose tolerance test (OGTT): This test measures blood sugar levels before and two hours after drinking a sugary drink. A blood sugar level of 200 mg/dL or higher after two hours is indicative of diabetes.
- Haemoglobin A1C test: This test measures average blood sugar levels over the past two to three months. A level of 6.5% or higher is indicative of diabetes.
- Random plasma glucose test: This test measures blood sugar levels at a random time. A level of 200 mg/dL or higher, along with symptoms of diabetes, is indicative of diabetes.
How to diagnose gestational diabetes
Gestational diabetes is typically diagnosed through a glucose screening test and a follow-up glucose tolerance test. Here's how the process usually works:
- Glucose screening test: This test is usually done between 24 and 28 weeks of pregnancy. The test involves drinking a sugary drink and then having blood drawn one hour later. If the blood sugar level is 140 mg/dL or higher, the individual will need to proceed to a glucose tolerance test.
- Glucose tolerance test: This test is usually done after an overnight fast. The individual will drink a sugary drink, and then have blood drawn every hour for three hours. If two or more of the blood sugar levels are higher than normal, the individual will be diagnosed with gestational diabetes.
PREVENTION OF DIABETES
While it's true that Type 1 and Type 1.5 diabetes cannot be prevented since they result from issues with the immune system. And some causes of Type 2 diabetes such as age and genetic predisposition are beyond your control as well. However, there are many other factors that increase your risk of diabetes, which you can manage.
- Maintain a healthy weight: Being overweight or obese is a major risk factor for diabetes. Losing weight and maintaining a healthy weight through a combination of healthy eating and regular physical activity can help reduce your risk.
- Engage in regular physical activity: Regular exercise can help improve insulin sensitivity, which can reduce your risk of developing diabetes. Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week, spread out over at least three days.
- Eat a healthy diet: Focus on eating a diet that is rich in whole grains, fruits, vegetables, lean protein, and healthy fats. Limit your intake of processed foods, sugar-sweetened beverages, and saturated and trans fats.
- Quit smoking: Smoking can increase your risk of developing diabetes, so if you smoke, consider quitting.
- Limit alcohol consumption: Excessive alcohol consumption can increase your risk of developing Type 2 diabetes.
- Get regular check-ups: Regular check-ups with your healthcare provider can help identify any potential risk factors for diabetes, as well as help catch and treat diabetes early on.
DIABETES IN PREGNANCY
Gestational diabetes or diabetes in pregnancy occurs in about 7% of all pregnancies, according to the American Diabetes Association. It usually develops around the 24th to 28th week of pregnancy and is caused by hormonal changes. During pregnancy, the placenta produces hormones that can make it harder for the mother's body to use insulin effectively, leading to gestational diabetes.
Pre-gestational diabetes
Pre-gestational diabetes refers to Type 1 or Type 2 diabetes that is present in a woman before she becomes pregnant. Women with pre-gestational diabetes who become pregnant have an increased risk of complications for both themselves and their babies.
Risks to your newborn
When a mother has diabetes, high blood sugar levels can cross the placenta and cause the baby's pancreas to produce more insulin. This can lead to several complications for the baby, such as:
- Macrosomia: This refers to a larger-than-average birth weight, which increases the risk of delivery complications such as shoulder dystocia and cesarean delivery.
- Hypoglycemia: The baby's blood sugar levels may drop rapidly after birth, leading to hypoglycemia or low blood sugar.
- Respiratory distress syndrome (RDS): Babies born to mothers with diabetes are at increased risk of RDS, a condition where the baby's lungs are not fully developed, and they have difficulty breathing.
- Jaundice: Babies born to mothers with diabetes are at increased risk of developing jaundice, a condition where the baby's skin and eyes turn yellow due to high levels of bilirubin in the blood.
- Birth defects: Poorly controlled blood sugar levels during pregnancy can increase the risk of birth defects, such as neural tube defects and congenital heart defects.
Does gestational diabetes disappear on its own?
Gestational diabetes typically resolves on its own after the baby is born. Once the baby is born, the placenta is also removed, and hormone levels return to normal, which can help the mother's body regulate blood sugar levels.
After delivery, healthcare providers will typically monitor the mother's blood sugar levels to ensure they return to normal levels. In some cases, blood sugar levels may remain high after delivery, indicating that the mother may have had undiagnosed type 2 diabetes before pregnancy or developed it during pregnancy. In these cases, ongoing treatment and management of diabetes may be necessary.
DIABETES IN CHILDREN
Although the prevalence of Type 2 diabetes in children is not as high in India as it is in Asian countries like Japan, cases of Type 2 diabetes in children are gradually increasing across the country. In 2018, referral centres such as Lucknow and Chennai reported that the proportion of children with Type 2 diabetes was 12% and 26.7%, respectively. The incidence of Type 1 diabetes mellitus (T1DM) is also on the rise, although not as rapidly as Type 2 diabetes. The prevalence of Type 1 diabetes is increasing at a rate of 3-5% per year in India.
Type 1 diabetes
This is the most common type of diabetes in children. It occurs when the immune system attacks and destroys the cells in the pancreas that produce insulin, a hormone that helps regulate blood sugar levels. Without enough insulin, glucose builds up in the bloodstream, leading to high blood sugar levels. Type 1 diabetes is usually diagnosed in children and young adults, and there is no cure. Children with type 1 diabetes require daily insulin injections or the use of an insulin pump to manage their blood sugar levels.
Type 2 diabetes
This type of diabetes is becoming increasingly common in children, particularly those who are overweight or obese. Type 2 diabetes occurs when the body becomes resistant to insulin, and blood sugar levels remain high. This can lead to complications such as nerve damage, kidney disease, and heart disease. Treatment for type 2 diabetes in children typically involves lifestyle changes such as a healthy diet and regular exercise, along with medications or insulin therapy in some cases.
Symptoms of diabetes in children can include:
- increased thirst and urination
- Hunger
- Fatigue
- Blurred vision
- Slow healing of cuts or bruises.
Parents and caregivers of children with diabetes play a critical role in managing the condition, including monitoring blood sugar levels, administering insulin or medications as needed, and helping children make healthy lifestyle choices. If you suspect your child may have diabetes, it's important to see a healthcare provider for testing and diagnosis. Early diagnosis and treatment can help prevent complications and improve outcomes for children with diabetes. With proper management, children with diabetes can live healthy, active lives.
FINAL TAKEAWAY
In conclusion, diabetes is a chronic disease that affects millions of people worldwide. It is essential to understand the causes, symptoms, and treatments of diabetes to manage the condition effectively. If you suspect that you have diabetes or are at risk for diabetes, speak to your doctor for advice on how to manage the condition and maintain good health.